As a pelvic floor physical therapist, I talk about bowel movements on a DAILY basis. Whether my clients aren't going enough, are going to much, can't control when they go, and everything in between. I'm so used to talking about it that I've actually forgotten how uncomfortable it can make people. The funny thing is, people don't want to "like" a poop post, but everyone wants to learn more about it! So let me be your BM sherpa and explain some of the most common questions I get.
Let's dive right in!
Digestion 101
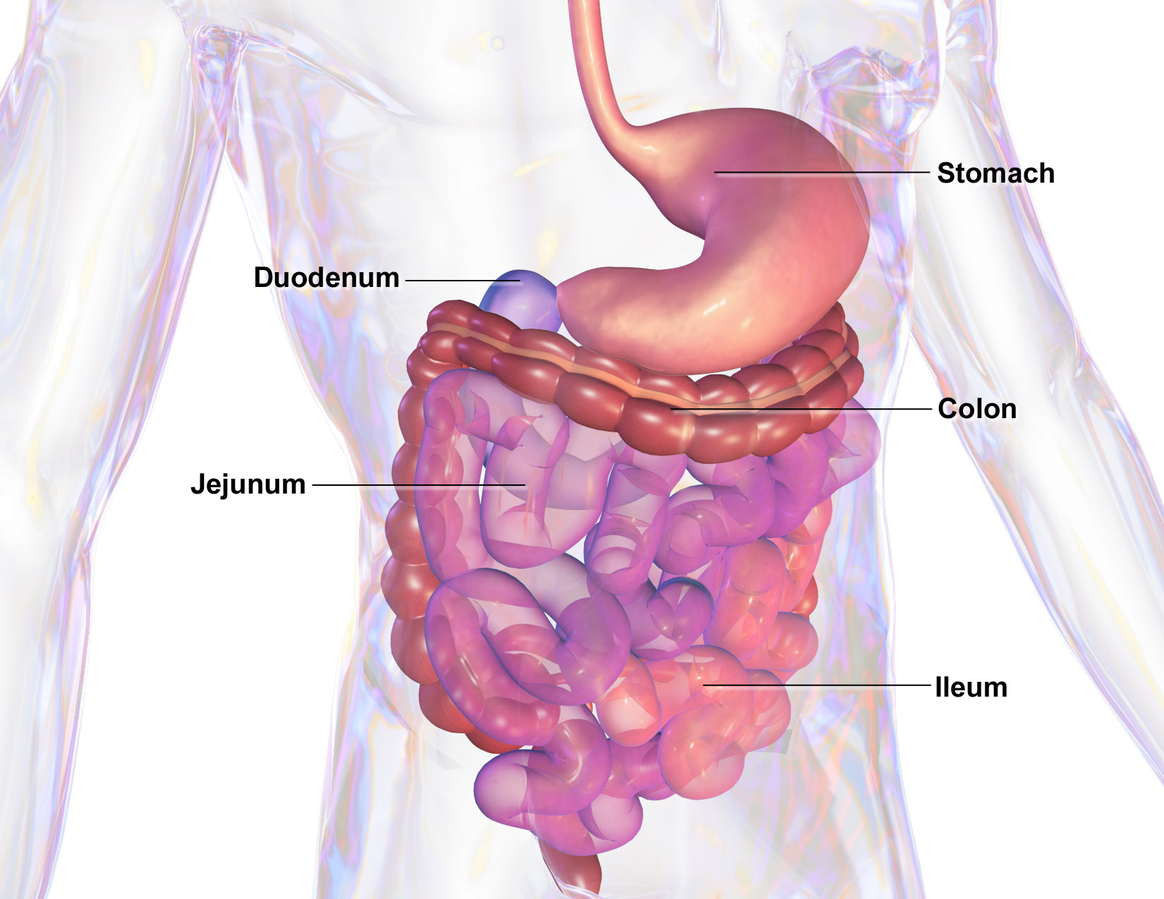
Before you can poop, you have to have something to make that poop with! Once you eat a great meal, your body gets to work breaking down that food to pull out all the nutrients and fiber it can.
One key thing to understand about the digestive system is that it propels food along through involuntary contractions, know as peristalsis. This occurs all the way from the esophagus (the tube that connects your mouth to your stomach) through the intestines, all the way to the rectum, and finally out of your body. More on that later!
The digestive system is much more complex than just your stomach and intestines. Digestion starts when food enters your mouth. It gets broken down by chewing and through enzymes in the saliva.
Next, it travels down the esophagus and into the stomach where acids and (involuntary) contractions further break down the food.
From there, it travels into your small intestine, where nutrients are absorbed. This process takes between 4 to 6 hours. After the small intestine, what's left of the food passes into your large intestine, which reabsorbs water, sodium, and a few other nutrients. It can take from 24 to 72 hours to complete this process. This varies from person to person, and it's part of the reason why we can't tell everyone that they have to poop once a day.
From the large intestine, poop passes into the rectum and then out the anus. We’re gonna pause here for a second and give a big shoutout to the rectum. Not only is it subject to dirty jokes, but it's very under appreciated. The rectum is actually a highly advanced organ. There are special cells in the rectum which respond to stretch and identify whether the contents are solid, liquid, or gas. That's why you can tell when you have to fart versus have a bowel movement!
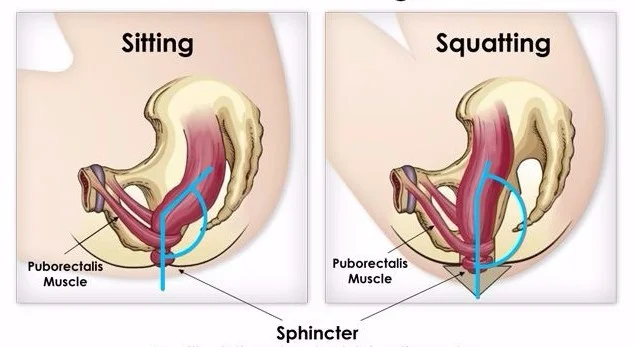
Remember those waves of peristalsis? Well that's what actually pushes poop out of your body! The external anal sphincter and puborectalis muscles are the key pelvic floor muscles when it comes to pooping. The picture below shows perfectly how the puborectalis muscles act as a sling around your rectum. This helps to keep you continent until you are able to get to the bathroom. When it's time to go, you need to relax these muscles, which loosens the sling and allows for complete emptying.
If needed, you could override the urge to go by holding a long pelvic floor contraction. HOWEVER you should not be overriding that urge on a regular basis!! Doing so for prolonged periods of time (think months to years) may extinguish the urge. Think of it like this. Your rectum is telling you “Hey, time to find a bathroom!” and you are always telling it “NOPE, not gonna happen.” Eventually, being the smart organ that the rectum is, it stops sending the traditional signal that you need to go. Desperate times call for desperate measures, and so the rectum starts to send more intense signals, such as pain or cramping to signal that you need to go instead.
Now on a more short term basis, if you defer the urge to poop until it's more convenient, say when you get home from work and try to go to the bathroom, you may rely on straining to try to start a bowel movement. While I get that being bloated and constipated are uncomfortable and even painful, straining is NOT an effective strategy to get things moving. Straining hard also typically results in contraction of the pelvic floor muscles, which makes it even LESS effective at actually passing a complete bowel movement! Chronic straining can weaken the pelvic floor muscles, nerves, and connective tissue. Not only that, but it can lead to hemorrhoids and pain.
If you have to strain to have a bowel movement, or you have pain with passing a bowel movement then you may have a pelvic floor muscle coordination issue. Good news, pelvic floor physical therapy can help you with that!
What's a normal poop?
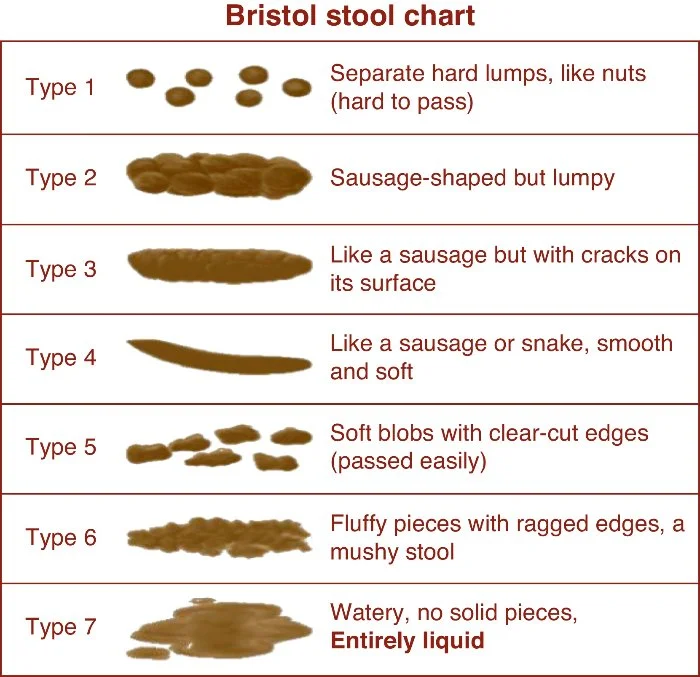
Now that we understand how the body forms feces, let's talk specifics. A normal frequency for bowel movements is anywhere between 3x/day up to 3x/week. More or less starts to become problematic. In addition to that, a normal bowel movement should also be a Type #3-4, as described on this lovely chart.
Yes, someone actually classified poop into different types but alas, that person was not me. *Cue sad violin music*
Types #1-2 are considered constipation and are associated with pain and difficulty passing. Types #5-7 indicate that feces are passing through you too quickly. Either of these could occur for many different reasons. An occasional bout of either due to a specific cause (i.e. a 24 hour stomach bug or constipation on that first day or two of travel) are nothing to stress over. However, if your normal is #1-2 or #5-7 then it's time to bring it up to your healthcare provider.
Ideal pooping position
Perhaps you’ve heard of the Squatty Potty? The reason it works so well is because it helps the puborectalis muscles relax. If you don’t want to go out and getting a pooping prop, then consider using a stool to help your stool.
Sorry, I just can’t resist the puns! What's most important is that your knees are above your hips. You do need to have your feet supported on something so that your body is relaxed. While squatting certainly meets the goal of knees higher than hips, most people from sedentary cultures can’t relax in this position. In the United States, the years of sitting to poop and sitting for many daily activities has turned the deep squat into an active exercise, not a position of relaxation. Remember, hovering in a squat over the toilet automatically turns your pelvic floor muscles ON which is the opposite of what you want!
A pelvic floor physical therapist's guide for potty training.
Notice that I didn't specify who this guide should be used for... because these same rules apply for toddlers, geriatric folk, and anyone in between! Obviously the way you apply it may very depending on your audience.
- Do respect the urge to go. When your body gives you the urge, those waves of peristalsis are doing their thing and you are most likely to have a well formed, easy to pass bowel movement. Unless you are physically unable to get to the bathroom, you need to respect this urge and go! I promise being a couple minutes late is not the end of the world. If your little one tells you he or she has to go, then get get him or her to the bathroom!
- Don’t sit on the toilet forever. If you don’t go within 5-10 mins, then get off the toilet. Contrary to popular belief the toilet is not the place to check a week's worth of emails or your Facebook feed. If nothing's happening then go about your daily business till that next urge comes along.
- DON’T strain!! Remember, the pelvic floor needs to RELAX when you are having a bowel movement. This is especially key for ladies - the female pelvic floor is anatomically more susceptible to damage from years of chronic straining. This can also contribute to hemorrhoids and rectal prolapse. When you're on the toilet, you should always focus on RELAXING.
- Eat good food! This is especially key for children. Studies have found that the foods which are available at home are the strongest predictor for what foods children will eat. Logically, this seems like it would be true for us adults too. You aren't going to have a big bowl of veggies if the only thing you have at home are Ramen noodles. Eating healthy, balanced meals is going to help you poop, feel more energized, less bloated, and contribute to numerous other benefits!
Enjoyed this post? Check out 6 Ways to Have a Better #2.
Resources
- Pelvic Physical Therapy Level 2 Management of Pelvic Pain and Defacatory Disorders: A Case Based Approach. Brooks Rehab, Institute of Higher Learning. August 2016.
- Parental Influence on Eating Behavior. Sept 2008. Published in the Journal of Law, Medicine, and Ethics. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2531152/